Good News for Families Navigating Cyclic Vomiting Syndrome (CVS)!
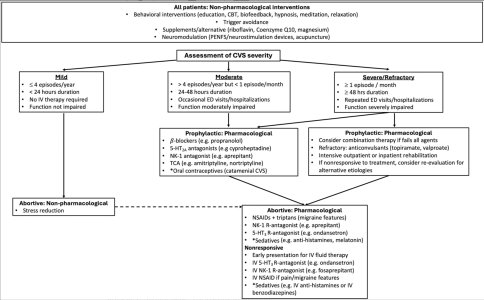
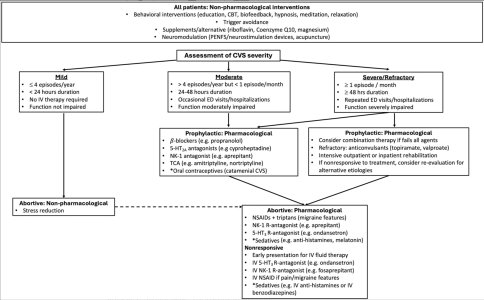
We’re excited to share brand-new 2025 clinical guidelines from the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition — and they include hopeful, low-risk strategies for managing CVS in children.
Here are some practical, non-medication options you can try at home — especially if your child is sensitive to medications or you prefer holistic approaches:
Abortive Interventions (When an Episode Starts):
Mind-body therapies like neuromodulation, acupuncture, and behavioral interventions can be helpful during acute episodes — especially for kids who don’t tolerate meds well. These are safe, gentle options worth trying in collaboration with your care team.
Topical capsaicin (yes, like chili peppers!) might also help, based on its use in similar conditions.
Prevention Tips That Are Easy to Implement:
Prioritize sleep – Consistent and quality rest is a known protective factor against CVS attacks.
Be mindful of common triggers like fasting, dehydration, stress, overexertion, and certain foods — even though the research isn’t clear-cut yet, some families find avoiding these helps.
Supplements That May Help (Talk to Your Doctor First!):
Coenzyme Q10 – Can be tried for 3–6 months to see if it reduces episodes. Be aware of cost and varying product quality.
Riboflavin (Vitamin B2) – Higher doses, taken twice daily, have shown promise in kids with migraines and may benefit those with CVS too.
Magnesium – Choose forms like magnesium glycinate, which are easier on little tummies and less likely to cause diarrhea.
L-carnitine is not recommended unless used in combo with CoQ10, and only under medical supervision.
Whole-Child Approaches Also Recommended:
- Psychological therapies
- Lifestyle coaching
- Routines and consistent treatment plans
These nonpharmacological tools are low-risk and empower families to take a proactive role — especially when used in partnership with your medical provider.
Source:
North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition
Published April 14, 2025 – Read the study here
 Let us know: Have you tried any of these approaches? What’s worked for your child? Share your journey in the comments or our support forum
Let us know: Have you tried any of these approaches? What’s worked for your child? Share your journey in the comments or our support forum
We’re excited to share brand-new 2025 clinical guidelines from the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition — and they include hopeful, low-risk strategies for managing CVS in children.
Here are some practical, non-medication options you can try at home — especially if your child is sensitive to medications or you prefer holistic approaches:
Abortive Interventions (When an Episode Starts):
Mind-body therapies like neuromodulation, acupuncture, and behavioral interventions can be helpful during acute episodes — especially for kids who don’t tolerate meds well. These are safe, gentle options worth trying in collaboration with your care team.
Topical capsaicin (yes, like chili peppers!) might also help, based on its use in similar conditions.
Prevention Tips That Are Easy to Implement:
Prioritize sleep – Consistent and quality rest is a known protective factor against CVS attacks.
Be mindful of common triggers like fasting, dehydration, stress, overexertion, and certain foods — even though the research isn’t clear-cut yet, some families find avoiding these helps.
Supplements That May Help (Talk to Your Doctor First!):
Coenzyme Q10 – Can be tried for 3–6 months to see if it reduces episodes. Be aware of cost and varying product quality.
Riboflavin (Vitamin B2) – Higher doses, taken twice daily, have shown promise in kids with migraines and may benefit those with CVS too.
Magnesium – Choose forms like magnesium glycinate, which are easier on little tummies and less likely to cause diarrhea.
L-carnitine is not recommended unless used in combo with CoQ10, and only under medical supervision.
Whole-Child Approaches Also Recommended:
- Psychological therapies
- Lifestyle coaching
- Routines and consistent treatment plans
These nonpharmacological tools are low-risk and empower families to take a proactive role — especially when used in partnership with your medical provider.
Source:
North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition
Published April 14, 2025 – Read the study here
Last edited: