Does constipation go away after stopping gluten in newly diagnosed celiac disease pediatric patients?
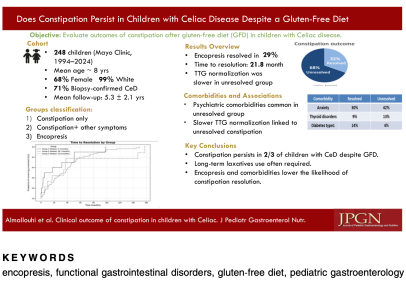
A 2025 study in Journal of Pediatric Gastroenterology & Nutrition followed 248 children with celiac disease who initially presented with constipation.
The findings were striking:
• Only 32% had constipation fully resolve on a gluten-free diet
• 68% required ongoing laxatives, even years later
• Children with encopresis had even lower resolution rates
• Anxiety, depression, and thyroid conditions were more common when constipation persisted
Bottom line: a gluten-free diet alone is often not enough. Constipation in children—especially when chronic—requires long-term, multidisciplinary support, not just dietary changes.
Source: Almallouhi A, Sadek M, Absah I. Clinical outcome of constipation as the presenting symptom in children with celiac disease. J Pediatr Gastroenterol Nutr. 2025. doi:10.1002/jpn3.70316
#PediatricGI #CeliacDisease #ChildhoodConstipation #Encopresis #GutHealthKids #ParentSupport #MyLittleTummyAches #EvidenceBasedParenting
A 2025 study in Journal of Pediatric Gastroenterology & Nutrition followed 248 children with celiac disease who initially presented with constipation.
The findings were striking:
• Only 32% had constipation fully resolve on a gluten-free diet
• 68% required ongoing laxatives, even years later
• Children with encopresis had even lower resolution rates
• Anxiety, depression, and thyroid conditions were more common when constipation persisted
Bottom line: a gluten-free diet alone is often not enough. Constipation in children—especially when chronic—requires long-term, multidisciplinary support, not just dietary changes.
Source: Almallouhi A, Sadek M, Absah I. Clinical outcome of constipation as the presenting symptom in children with celiac disease. J Pediatr Gastroenterol Nutr. 2025. doi:10.1002/jpn3.70316
#PediatricGI #CeliacDisease #ChildhoodConstipation #Encopresis #GutHealthKids #ParentSupport #MyLittleTummyAches #EvidenceBasedParenting
Attachments
Last edited: